Diabetes distress is a common occurrence in people diagnosed with diabetes.1 It is defined as an emotional response characterised by extreme apprehension, discomfort or dejection, due to perceived inability in coping with the challenges and demands of living with diabetes.2 Women with gestational diabetes have been reported to use various coping strategies to address the stress.3, 4 These include both healthy (effective) and unhealthy (ineffective) coping strategies. Those with planned pregnancy, a high educational level, or a first pregnancy coped effectively with stress during pregnancy. Those who were unemployed and had a second or subsequent pregnancy coped ineffectively with stress during pregnancy.5 Pregnant women with gestational diabetes mellitus are less likely to use the effective coping styles as compared to healthy pregnant women.6 The importance of using effective coping skills by pregnant women is highlighted by the fact that it is associated with better glycaemic control as reflected by glycated haemoglobin (HbA1c) levels.5
Coping-skills training is therefore a recommended management strategy for diabetes distress.2,7 In order to effectively administer coping-skills training one must begin by analysing the current coping styles of the individual.8 The GlucoCoper is a brief, simple, easy-to-administer tool for assessing the coping mechanism of people with diabetes mellitus.2 The tool has been validated in a large single-centre study in adults with type 2 diabetes.9 The GlucoCoper offers a salutogenic assessment of coping in diabetes, and is significantly shorter and easier to use as compared to other existing tools. The instrument is developed so as to be useful in both busy clinical practice as well as in research settings.
Pregnancy is a state of increased vulnerability among women diagnosed with diabetes. This puts them at an increased risk of experiencing psychosocial ill health, including diabetes distress.10,11 Hence, there is a need to assess coping skills in women with pregnancy complicated by diabetes.
Aim
The current study aimed at assessment of feasibility of using the GlucoCoper as a screening tool. Additionally, we compared the performance of the GlucoCoper with the Hyperglycemia in Pregnancy Distress Scale (HyPreDS) – a 15-item instrument used to assess diabetes distress during pregnancy.9 We also explored the possibility of creating a briefer version of the GlucoCoper, with an aim to reduce assessment time even further.
Table 1: Hyperglycaemia in pregnancy distress scale

Participants were required to rate the statements by writing 1, 2, 3, 4, 5 options according to criteria as given below
Material and methods
This was an exploratory, cross-sectional, observational study carried out at a single centre. The GlucoCoper was administered to women diagnosed with diabetes seeking consultation from an antenatal care facility of an endocrinology centre in Karnal, Haryana, India. All pregnant women seeking antenatal care from the treatment centre were approached for participation in the study. Informed, written consent was sought, and those who refused consent for participation in the study were excluded. Women with other co-morbid medical disorders were excluded. Similarly, those who were engaged in the care of another family member with a chronic illness were excluded. Details of the socio-demographic profile were gathered using a semi-structured proforma. It included variables such as age, family income, duration of diabetes, were recorded. HbA1c levels were recorded based on the most recent report available with the study subject.
All the subjects were administered the HyPreDS (Table 1). The HyPreDS is a 15-item, 5-point Likert scale-based questionnaire used to assess diabetes distress in antenatal women with diabetes. It is divided into three domains: concern for unborn child health, concern for self-health, and concern for social health. The coping styles were assessed using the six-item GlucoCoper. The GlucoCoper is a brief, simple, easy-to-administer tool for assessing the coping mechanisms of people with diabetes mellitus.2 It has been developed by a multi-disciplinary team comprising of an endocrinologist, psychiatrist, psychologist, diabetes educator and gynaecologist. The GlucoCoper includes six items rated on a graphic 10-point Likert scale. These include four items to assess positive coping skills (acceptance, optimism, planning and action) and two items to assess negative coping mechanisms (negativity and blame). Adding the score of the four items aimed at assessing the positive coping mechanisms derives the total positive coping sub-scale score, and adding the score of the two items aimed at assessing the negative coping mechanisms derives the total negative coping sub-scale score. The total score on the GlucoCoper is derived by adding the scores of the positive and negative sub-scale scores. The assessments were completed in a single session.
Table 2: Mean scores on GlucoCoper

SD = standard deviation
Statistical analysis
Data were analysed using SPSS version 16. Pearson Product-Moment correlations were computed to examine correlations between distress and coping dimensions and socio-demographic (age, income) and clinical (HbA1c, duration of diabetes mellitus) variables. Percentile ranks were calculated for determination of cut-off scores for each coping dimension.
Table 3: Pearson Product-Moment correlations of positive and negative coping
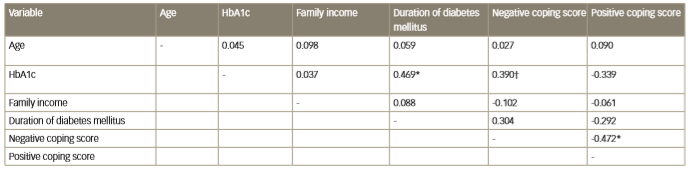
* Correlation is significant at the 0.01 level (2-tailed)
† Correlation is significant at the 0.05 level (2-tailed)
HbA1c = glycated haemoglobin
Table 4a: Correlations of distress scale in pregnancy with negative coping

* significant at 0.05 level
† significant at 0.01 level
HIP = Hyperglycaemia in pregnancy
Table 4b: Correlations of distress scale in pregnancy with positive coping

* significant at 0.05 level
† significant at 0.01 level
HIP = Hyperglycaemia in pregnancy
Results
A total of 30 subjects were included in the current study. Of the 30 participants, 18 were graduates or post graduates and 12 had completed 12 years of schooling. The majority (n = 21) belonged to urban families, while nine were from a rural background. Seven participants had type 1 diabetes, 12 had pre-existing type 2 diabetes, and 11 were diagnosed as having gestational diabetes mellitus.
The mean score of the study subjects on the six-item GlucoCoper has been presented in Table 2. The total GlucoCoper score was calculated by taking the total of the four positive skills, and subtracting the scores of the two negative mechanisms. Negative and positive coping scores correlated inversely with each other (r = 0.472, p < 0.05; Table 3). Duration of diabetes correlated positively with HbA1c (r=0.469, p<0.05). Age, family income and duration of diabetes did not correlate significantly with the positive or negative coping scores (Table 3). When individual coping skills were analysed, duration of diabetes was found to correlate negatively with optimism (r=0.430, p=0.05). HbA1c was found to be positively correlated with negativity (r=0.39, p<0.05), and also correlated negatively with planning (r=0.46, p<0.01). Highly educated subjects revealed greater negativity, while those from a rural background exhibited higher blame scores of ≥7.00 for negativity, ≤4.00 for planning, and ≤5.00 for action.
The correlation of the GlucoCoper with the HyPreDS was also assessed (Table 4). Seven items of the HyPreDS were found to correlate significantly with negative coping (Table 4a), while eight demonstrated a significant negative correlation with positive coping (Table 4b). Negative coping correlated with four concerns related to social health (extra expense, not being allowed to eat properly, lack of acceptance by in-laws, and blame being placed on parents), two concerns related to self-health (permanent dependence on insulin, obstetric complications), and one item related to concern for unborn child’s health (admission in nursery). The eight items which correlated negatively with positive coping included all five concerns related to social health, one concerned with self-health (obstetric complications) and two linked to the unborn child’s health (pregnancy loss, admission in nursery). These items are related more to immediate health concerns, rather than to health issues which may occur in the distant future.
Negativity (R=-0.421), planning (0.642) and action (0.625) were the three domains which correlated strongly with the GlucoCoper score. Hence, further statistical analysis was performed using these three scores. Cut-offs were determined for each of these three scores using Tukey’s hinges. A 75th percentile score was considered high, while 50th and 25th percentile scores were graded as moderate and low, respectively. Based upon this, a negative score of ≥7.00 was classified as high, while ≤4.00 was considered low. Similar cut-offs for planning were ≥7.00 and ≤4.00, and for action were ≥8.00 and ≤5.00 respectively. Thus, a brief three item GlucoCoper can be used to screen for coping mechanisms in pregnancy complicated by diabetes. Coping scores of ≥7.00 for negativity, ≤4.00 for planning, and ≤5.00 for action can be considered dysfunctional.
Discussion
Diabetes distress and dysfunctional coping mechanisms are two sides of the same coin. The current study has tried to analyse correlates of dysfunctional coping, which in turn, may influence severity of diabetes distress. The focus population of this study, i.e., antenatal women, is extremely important. Glycaemic control during pregnancy influences not only maternal health and well-being, but also impacts post-partum metabolic health of the women concerned, and long-term health of the unborn foetus.9-11 Mitigation of diabetes distress is an important aspect of diabetes care.12,13 Hence, it is necessary to study the correlates of coping with such stress during pregnancy.
The results of this study reveal useful insights. HbA1c was found to be positively related with negative coping, and longer duration of diabetes correlated negatively with optimism, reinforcing the bidirectional link between hyperglycaemia and psychological morbidity. Negative coping in educated women may be due to greater awareness of potential risks of a diabetic pregnancy. The lack of planning and action exhibited by women from rural background may be a reflection of prevailing societal mores which keep women in a passive and inactive mode.13
Positive coping skills were inversely correlated with all five items of the Social Health domain of the HyPreDS. This implies that once social concerns set in, the person loses the capacity to exhibit positive coping skills. It may also suggest that women with lack of positive skills are more prone to social ill-health. A similar negative correlation of positive coping was seen in women who report concern for pregnancy loss, and concern for neonatal or obstetric outcomes. Such concern may be a cause of, or an effect of, inadequate positive coping.
Negative coping was found to correlate positively with various items on the HyPreDS, including concern for obstetric complications, concern about dependence on insulin, concern about neonatal admission in nursery, and concern for social health. The high correlations between various positive skills, between the negative skills, and the inverse correlation between positive and negative skills suggests a high degree of internal validity. The association between coping and pregnancy-specific distress has been reported in high-risk pregnant women.14–17 Distress levels relate to preterm delivery, physical symptoms, labour and delivery, weight gain, and having an unhealthy baby. Coping is carried out through prayer and positive appraisal. Coping by avoidance, preparation for motherhood, and substance use is associated with greater distress, while positive appraisal is associated with less distress.14,15 Our results strengthen earlier reports,17 and add to their utility by suggesting that the GlucoCoper can be used not only as a tool to assess coping mechanisms, but also as a surrogate means of screening for diabetes distress in pregnancy. Depending upon the healthcare system environment, availability of manpower and time, and clinical situation, the GlucoCoper can be administered as a stand-alone screening/diagnostic instrument, in conjunction with the HyPreDS, or after the HyPreDS has revealed significant distress.
The three-item GlucoCoper provides a simpler tool which can be used to screen for dysfunctional coping skills. The cut-offs of ≥7.00 for negativity, ≤4.00 for planning, and ≤5.00 for action may be taken as thresholds for further diagnostic and therapeutic action. Such scores should prompt screening for diabetes distress, and suggest the need for coping-skills training in affected women. Either the six-item GlucoCoper or the three-item brief GlucoCoper can be used to screen for dysfunctional coping, and for concomitant diabetes distress in pregnancy. The GlucoCoper can be used before, after, or in conjunction with the Diabetes Distress Scale.
Our study does have limitations, including its single-centre characteristic, the small sample size, and lack of correlation with other diabetes distress measuring instruments such as the Diabetes Distress Scale.12 The HYPredDS has not been validated prior to this study, either. However, in view of the paucity of data in this important field of obstetric medicine, our results assume great significance. Our data are concordant with that of authors from Italy and Ireland,17,18 who report poor quality of life, and a high level of diabetes distress, in type 1 and gestational diabetes mellitus.13,14














