Data from the INTERHEART study, a case-control study involving participants from 52 countries, also indicate that nine traditional factors may account for as much as 90% of population-attributable risk for myocardial infarction in men and 94% in women.1 However, these figures should be interpreted with care and considered as rough estimates of a preventative potential embedded in the listed risk factors, and do not necessarily say anything about causal relationships.2,3 Furthermore, case-control studies tend to inflate the impact of risk.
Data from the INTERHEART study, a case-control study involving participants from 52 countries, also indicate that nine traditional factors may account for as much as 90% of population-attributable risk for myocardial infarction in men and 94% in women.1 However, these figures should be interpreted with care and considered as rough estimates of a preventative potential embedded in the listed risk factors, and do not necessarily say anything about causal relationships.2,3 Furthermore, case-control studies tend to inflate the impact of risk. Still, we need further improvements in risk prediction techniques and a better understanding of the basic mechanisms behind occurrences of cardiovascular disease. Certain events cannot be explained by the common risk factors.
Genetic Markers of Cardiovascular Disease
The rapid advances within genetics and vascular cell biology and atherosclerosis research have directed recent research interest towards the clinical usefulness of genetic factors as well as measurable biochemical and immunological markers. The INTERHEART study did not provide data on familial factors or novel biomarkers. It is well known that cardiovascular disease (CVD) and particularly coronary heart disease (CHD) runs in families. Long-term follow-up studies on the Swedish Twin Registry indicate that genetic influences are particularly important for premature death from CHD,4 and furthermore that heritability estimates indicate that the risk of dying from CHD can partly be attributed to genetic factors, with a heritability of 57% for men and 38% for women.5 The genetic influences on death from CHD were mediated through common risk factors to a greater extent among women than men.5 During recent years, several potentially important genes for CHD and myocardial infarction (MI) have been identified, applying various candidate gene approaches6 for the genes stromelycin-1 (5A-1171/6A), a metalloproteinase of the arterial wall,7 ALOX5AP and LTA4 in the leukotriene pathways8,9 and TNFSF4 of the Ox40L, a pro-inflammatory cytokine,10 to mention just a few of the most challenging genes. The problems have been to confirm and replicate initial findings, most likely due to variations in study designs, end-point classifications and difference in population structures. However, more recent replications have been more successful through large-scale genome-wide associations by which novel chromosomal regions such as 9p21 have been identified and also related to CHD without being linked to traditional risk factors.11,12 The prospects for these huge undertakings look promising, particularly with regard to unravelling novel mechanistic pathways, creating data for analyses of gene–environmental interactions and exploring potential routes towards the development of prodrugs, but the clinical utility for risk prediction remains to be seen. Biomarkers at Various Stages of the Vascular Process Towards a Cardiovascular Event
Evidence from experimental and clinical research indicates a central role of low-grade inflammation in CHD and the development of atherosclerosis.13,14 Early on in the atherosclerosis process, immune cells are important players. Inflammatory cytokines stimulate endothelial adhesion molecules and, furthermore, the production of interleukin 6 (IL-6), which in turn stimulates the liver to produce acutephase reactants such as C-reactive protein (CRP). Macrophages are essential in the atherosclerosis process with the uptake of oxidised low-density lipoprotein (OxLDL) into the atherosclerotic plaques. There is a fine-tuned interplay between various markers and activators, leading to the development of atherosclerotic lesions that eventually may rupture with severe clinical consequences. So, the question is whether circulating markers may reflect the vascular processes in a sufficiently reliable way to permit cardiovascular risk prediction.
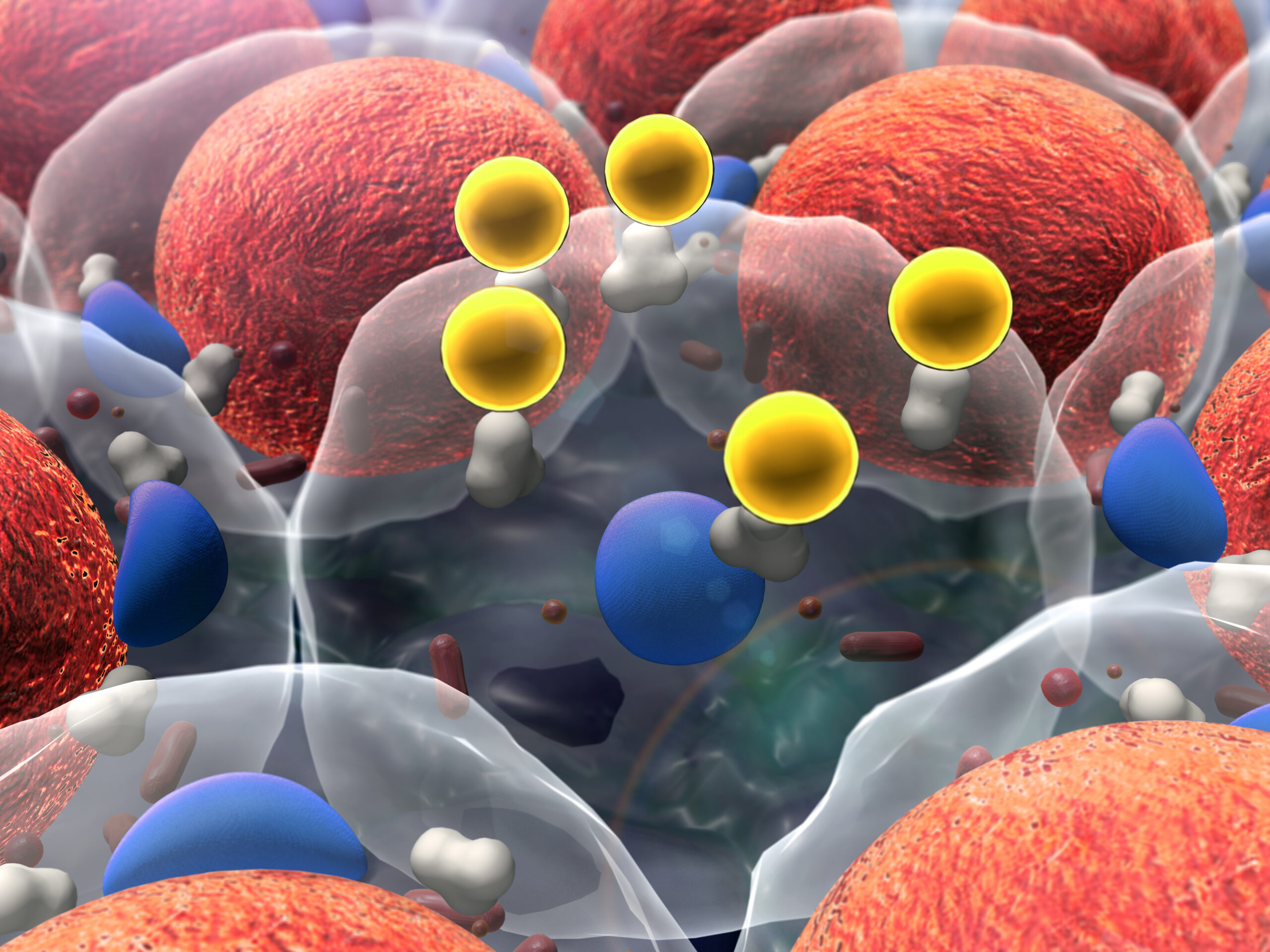
The significance of the various biomarkers may differ throughout the course of a vascular process with genetic, inflammatory and immunological markers acting early on in the process. It is possible, though, that inflammatory/immunological factors are also related to plaque instability and prognosis once myocardial damage has occurred. Abbreviations used for the various biomarkers are explained in the text.
A number of serum- or plasma-based biomarkers have been used to determine cardiovascular risk independently of the common risk factors (see Figure 1). Several biomarkers can be considered to be determinants of risk and/or prognosis for CVD events. Some of the novel biomakers are causally related to cardiovascular events and the underlying vascular processes, such as certain genetic polymorphisms. Some of the inflammatory biomarkers are also most likely causally related to cardiovascular diseases such as OxLDL, antibodies against phosphorylcholine (anti-PC) and lipoprotein-associated phospholipase A2 (LpPLA2), whereas other inflammatory biomarkers such as CRP and myeloperoxidase (MPO) are most likely only markers of an activated ongoing low-grade inflammation and are not necessarily causally related risk factors. Plasma D-dimer, a fragment generated from fibrin during lysis of clots in vivo, does not seem to add predicted information above that of plasma fibrinogen, a prothrombotic factor related to the degree of low-grade inflammation.15 The independent roles of these pro-thrombotic factors have not been reliably settled and they should not be considered as risk factors, but instead as risk markers.16 The importance of plaque ruptures as initiators of acute coronary syndromes (ACS) and MIs have been highlighted during recent years. Many of the inflammatory markers as well as the traditional risk factors may be implicated in plaque instability.13,14However, special interest has been directed towards factors more directly related to stability of the atherosclerotic lesions such as metalloproteinases and, particularly, MMP-9 and pregnancy-associated plasma protein-A (PAPP-A), but their predictive roles are still not fully known.17,18 The cardiac natriuretic peptides brain natriuretic peptide (BNP), N-terminal probrain natriuretic peptide (NT-proBNP) and atrial natriuretic peptide (ANP) are secreted by the heart in relation to increased transmural pressures. These have been used to test for early signs of heart failure19 and may add prognostic information once a cardiac event has occurred (and probably also in healthy subjects).20,21 Sensitive markers for myocardial damage such as creatine kinase-MB (CKMB), cardiac troponin 1, myoglobin and heart-type fatty-acid-binding protein (HFABP) provide information on prognosis and can be used for early risk stratification of patients with unstable angina.22–24 Troponin I has also been shown to predict death and first CHD events in healthy men, indicating the importance of silent cardiac damage for predicting outcome in the general population.25
Own preliminary data indicate that anti-PC binds to the PC epitope on OxLDL and blocks the macrophage uptake of OxLDL, and thereby also blocks plaque formation.
Oxidised Low-density Lipoprotein and Antibodies Against Phosphorylcholine
Markers related to the inflammatory vascular processes are attracting an increased interest. Oxidised stress leading to the formation of OxLDL is of importance for both initiation and progression of the atherosclerotic process. Enzyme-linked immunosorbent assays (ELISAs) to measure circulating OxLDL are commercially available, and crosssectional data suggest a relationship with CHD, but its role as a risk predictor is still unclear.26 Elevated levels of autoantibodies against OxLDL have been found in patients with carotid atherosclerosis and peripheral vascular disease,27,28 and elevated levels could also predict MI over 10–20 years of follow-up in healthy 50-year-old men.29 OxLDL also has pro-inflammatory and immunogenic properties30,31 and contains other oxidised products including platelet activating factor (PAF)-like lipids, where phosphorylcholine (PC) is the main epitope.32–34 PC is necessary for binding to the PAF-receptor and, in addition, other pro-inflammatory effects of OxLDL could be caused by PAF-like lipids.32–35 PC is also a component of some bacteria and apoptotic cells, and thus could be recognised by anti-PC antibodies.36 Antibodies against PC have been characterised as a natural antibody that can be produced in the absence of external antigens.37Such antibodies have been shown to prevent lethal infections with Streptococcus pneumoniae in mice.38Our own data on 226 patients with hypertension followed for four years with repetitive ultrasound measurements of carotid intima-media thickness imply that high antibody levels of the immunoglobulin M (IgM) subclass to PC and OxLDL are associated with less progression of intima-media thickness.39 A further study from our group (on 349 incident CVD events, CHD and ischaemic stroke and 693 age- and sexmatched controls identified over 12 years of follow-up from the Malmö-Diet Cancer Study) showed that with a new ELISA kit, CVDefine® (Athera Biotecnologies, Sweden) significant associations (independent of traditional risk factors) were noted with values below 17U/ml (corresponding to the lowest 9th percentile of the anti-PC distribution) and incident CVD (relative risk [RR] 1.79, 95% confidence interval [CI] 1.11–3.67).40 If men were studied separately the associations were somewhat attenuated. Among men the relationships were even more apparent for ischaemic stroke (RR 3.67, 95% CI 1.34–10.1). Confirmation and replication in other cohorts are necessary to be able to draw conclusions on causal mechanisms.
Preliminary data from a representative cohort on 60-year-old men and women from Stockholm support the findings from Malmö that low levels of IgM antibodies are related to an increased risk of suffering from CVD, particularly in men.41 However, it is still difficult to preclude the possibility of a risk relationship among women as well, as the number of female incident cases was fairly low. Analyses on other cohorts with higher numbers of incident MIs and stroke are under way, as are studies on short- and long-term prognosis after ACS. A consistent finding from our cohort materials39–41 has been that women have higher values of IgM antibodies against PC, a finding that may contribute to the lower burden of CVD in women.
Comparisons between native inhabitants from Kitava, New Guinea and participants from Sweden demonstrated higher antibody levels among New Guineans, a circumstance that may contribute to the low risks of CVD in this region of the world.42 The practical implications of our findings are yet not clear, but theoretically early identification of the highrisk groups susceptible for immunomodulation, either passively through polyclonal or monoclonal antibodies or actively through vaccination, could be an attractive mode of treatment. Experiments on knock-out mice with monoclonal IgM antibodies against PC have already shown that such therapies could stop atherosclerosis progression.43
Furthermore, active immunisation of such mice with PC or pneumococcal vaccine containing PC have also been shown to favourably affect atherosclerosis development.44,45 A potential mechanism behind the protective effects of high levels of IgM antibodies against PC could be our preliminary findings that these antibodies inhibit the uptake of OxLDL in monocytic cells differentiated into macrophages (see Figure 2).
C-reactive Protein
CRP is the most extensively studied inflammatory marker. More than 40 epidemiological cohort studies have been undertaken on associations between CRP and CHD, and on average the odds ratios corresponding to RR in the order of 1.6 (95% CI 1.5–1.7) have been obtained, associations of the same magnitude as for p-fibrinogen and triglycerides.46 Similar associations have also been found for risk of stroke.47 Some uncertainty still exists on the pathophysiological role of CRP because of its unclear relationship with the atherosclerotic process. CRP is positively related to several of the factors contained in the metabolic syndrome and inversely related to protective factors such as physical activity, high-density lipoprotein (HDL) cholesterol, apolipoprotein A1 and the consumption of fruits and vegetables.46Thus, the independent character of CRP has been questioned. Controversy also exists regarding its potential use as a risk marker in risk assessments. In guidelines from the American Heart Association (AHA)/Centers for Disease Control and Prevention (CDC) from 2003 on the prevention of cardiovascular disease, CRP was recommended for use at the discretion of the physician as part of a global coronary risk assessment in adults without known CVD48 (CRP was not recommended in Europe by the corresponding guidelines issued the same year).46 To further evaluate the causal role of CRP and CHD, large-scale multicentre studies are currently running applying a Mendelian randomisation technique to delineate possible significant associations between functional SNPs and haplotypes at the CRP locus influencing its circulating levels.50
In order to target possible interventional benefits from treatments with statins in subjects with elevated CRP levels, post hoc analyses were performed on randomised controlled trials in post-MI patients (Cholesterol Recurrent Events [CARE]) and a primary preventative study (Air Force/Texas Coronary Atherosclerosis Prevention Study [AFCAPS/TexCAPS]). Both of these studies suggested additional risk benefits by treatment with the statin in those with low LDL cholesterol but with elevated levels of CRP.51,52 These positive findings were confirmed by the results from the prematurely ended randomised placebo-controlled study Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER), a study on 17,802 healthy men and women with LDL cholesterol below 3.4mmol/l and hs-CRP levels above 2mg/l.53 LDL cholesterol was reduced by 50% and hs-CRP levels by 37%. The hazard ratio for the composite end-point (MI, stroke, arterial revascularisation, hospitalisation for unstable angina or death from CVD) was 0.56 (95% CI 0.46–0.69; p<0.00001). The encouraging data from this trial emphasise the possible impact of anti-inflammatory treatment in low-risk subjects with an activated low-grade inflammation. As the authors say, “Given the recognition that atherothrombosis is in some respects a disorder of innate immunity, we hope the data presented here spur the further development of targeted anti-inflammatory drugs as potential vascular therapeutic agents and lead to innovative trials that can directly address whether the inhibition of inflammation by agents other than statins can reduce the rates of vascular events.”
Lipoprotein-associated Phospholipase A2
Lipoprotein-associated phospholipase A2 (Lp-PLA2), an enzyme bound to LDL, hydrolyses oxidised phospholipids on OxLDL with the generation of pro-inflammatory products such as lysophosphatidylcholine and oxidised fatty acids.54 Furthermore, it can also hydrolyse PAF, another factor with pro-inflammatory properties. Lp-PLA2 is released from atherosclerotic lesions, particularly from more advanced lesions, which is why this enzyme may be related to
therosclerosis progression. Although not as well explored clinically and epidemiologically as CRP, the assembled information from over 10 cohort studies on both healthy subjects and patients with ACS and MI suggest that Lp-PLA2 might be related to both primary events (MI and stroke) as well as recurrences.54–58 However, as the number of participants in available studies has been too few to permit reliable risk estimates on subgroups of subjects and patients, an international collaborative meta-analysis will be performed; it is currently planned to include about 20 cohort studies with 15,000 CVD end-points.59
Recent data from the Malmö Diet Cancer study suggest that Lp-PLA2 is strongly correlated with several cardiovascular risk factors, particularly lipid fractions and also with degree of carotid atherosclerosis.60 Similarly, follow-up data from this cohort showed that Lp-PLA2 activity and mass were more related to risk of ischaemic stroke than CHD with multivariately adjusted RRs for activity measurements of 1.48 (95% CI 0.92–2.37) for CHD and 1.94 (95 % CI 1.15–3.26) for ischaemic stroke.61 Significant associations of the same magnitude were also noted for mass determinations with regard to incident stroke. The investigators from Malmö also found that Lp- PLA2 is associated with the metabolic syndrome and that elevated levels of Lp-PLA2 add prognostic information to the metabolic syndrome on incidence of cardiovascular events.62 Concluding Remarks
Currently, there is an intense search for novel cardiovascular biomarkers, and in parallel with these efforts the utility of novel players is under debate.2,3 Attempts to evaluate the incremental usefulness of multiple biomarkers have been made by the Framingham Heart Study (using 10 novel biomarkers) and the Atherosclerosis Risk In Communities (ARIC) study (using 19 novel biomarkers), in which novel biomarkers added only marginally to the traditional risk factors in predicting relative risks for major cardiovascular events and death and coronary heart disease.63,64 The majority of the novel biomarkers are to be considered as risk markers rather than risk factors as they do not convey independent predictive information once adjustments are made for traditional risk factors.
Recent analyses of associations between markers of inflammation and coronary artery calcifications (12 studies) usually show that positive associations disappear after adjustments for the presence of traditional risk factors.65 Also, the combined use of novel inflammatory markers may provide more informative data not only on prediction but also on mechanisms. The updated information on inflammatory biomarkers indicates that CRP seems to be the best general marker for an activated low-grade system inflammation, whereas Lp-PLA2 more directly reflects an activated vascular inflammation. Lp-PLA2 measurements have recently been recommended by an American panel as an adjunct to traditional risk assessments according to the Adult Treatment Panel III (ATP III) and AHA/CDC guidelines. So, despite the lack of data as from the JUPITER trial, the panel still recommends Lp-PLA2 as a diagnostic test for vascular inflammation to better identify patients at high or very high risk who should benefit from intensified lipid-modifying therapies.66 However, they do not recommend Lp-PLA2 as a target for therapy. As specific anti-CRP or anti-LP-PLA2 agents are unavailable, other more specific immunogenic biomarkers such as anti-PC could be of interest in the future. Data so far indicate that anti-PC values are not influenced by effects of metabolic risk factors in the way CRP and LP-PLA2 are. Furthermore, there are apparent links between the use of anti-PC and possible therapeutic alternatives such as immunomodulation of subjects with low levels of anti-PC, either through passive treatment with monoclonal antibodies or through vaccination.