Non-alcoholic fatty liver disease (NAFLD), actually the most common cause of chronic liver injury, comprises a disease spectrum ranging from simple steatosis to non-alcoholic steatohepatitis (NASH), advanced fibrosis and cirrhosis.1,2 NAFLD is defined as an accumulation of fat, mainly triglycerides (TG), in hepatocytes exceeding 5–10 % of the liver weight and this in the absence of significant alcohol consumption or any other cause of secondary liver steatosis or disease.3–5 NAFLD develops when fatty acid uptake and de novo fatty acid synthesis exceed fatty acid oxidation
Non-alcoholic fatty liver disease (NAFLD), actually the most common cause of chronic liver injury, comprises a disease spectrum ranging from simple steatosis to non-alcoholic steatohepatitis (NASH), advanced fibrosis and cirrhosis.1,2 NAFLD is defined as an accumulation of fat, mainly triglycerides (TG), in hepatocytes exceeding 5–10 % of the liver weight and this in the absence of significant alcohol consumption or any other cause of secondary liver steatosis or disease.3–5 NAFLD develops when fatty acid uptake and de novo fatty acid synthesis exceed fatty acid oxidation and export as triglyceride.6 NAFLD, often referred to as ‘simple steatosis’, appears to be a relatively uncomplicated form of chronic liver disease. A significant proportion of patients with NAFLD, however, progress to NASH. NASH is a much more serious form of chronic liver disease that includes inflammation and/or liver cell damage. In these patients fibrosis might develop, and patients can evolve to cirrhosis and its complications, including hepatocellular carcinoma.3,7,8
Data on the prevalence of NAFLD are limited by lack of an accurate, non-invasive screening tool in the general population.9 Ultrasound is useful for detecting steatosis, but cannot detect low grades of steatosis (<30 %) and cannot distinguish simple steatosis from NASH or fibrosis.10 Scoring systems based on laboratory parameters are insufficiently validated for the diagnosis of steatosis or NASH. Currently, a liver biopsy is the only definitive way to diagnose and stage NAFLD, particularly to differentiate simple steatosis from NASH.11 The invasive character of this procedure, however, limits its use on a large scale.9 Based on studies in relatively unselected populations, the prevalence of NAFLD is estimated to be approximately 20–30 %, this may rise to 75 % in an obese population.3,4,12,13 Approximately 10–25 % of NAFLD patients develop NASH. Progression of NASH to cirrhosis occurs in approximately 15–20 % of patients with NASH. Most patients with simple steatosis do not progress to NASH or cirrhosis.14
Metabolic syndrome, a complex condition linked to (intra-abdominal) obesity and characterised by insulin resistance, dyslipidaemia and hypertension,15 identifies individuals at high risk of both type 2 diabetes and cardiovascular disease.16,17 NAFLD is not included as a component of metabolic syndrome as it is currently defined; however, data suggest a potential association.2 Although the data are mainly from epidemiological sources, the pathogeneses of NAFLD and metabolic syndrome share common components, with the focus on insulin resistance as a key factor.11,18,19 The pathogenesis of NAFLD has to date not been completely elucidated, but might be partly related to a dysregulated cross-talk between liver and visceral adipose tissue (VAT).20 This article discusses the potential pathogenic link between VAT and fat accumulation in the liver.
Role of Visceral Adipose Tissue in Metabolic Disease in General
Not all obese individuals develop obesity-related metabolic cardiovascular disorders, potentially due to a preserved normal adipose tissue architecture and function.21 The majority of patients with obesity, however, have an impaired adipose tissue function caused by the interaction of genetic and environmental factors.22 Adipose tissue dysfunction may be considered as the cause of an accumulation of ectopic fat in liver, muscle and heart.
It is not yet clear whether visceral fat should also be considered to be a variant of this ectopic fat23 or as arising from an incapacity of the body to store fat in predesigned subcutaneous and/or gluteal areas.24 VAT is a sub-depot of total adipose tissue together with subcutaneous and intermuscular adipose tissue.25 Different methods are being used to assess the amount of visceral fat. Computed tomography (CT) has been considered to be the most accurate and reproducible technique.26 Other techniques used are magnetic resonance imaging (MRI)27 and ultrasonography.28 Waist circumference has been validated as an appropriate clinical substitute for CT.29 Studies have shown that adipose tissue is not simply a reservoir of energy which, by hydrolysis of TG, provides free fatty acids (FFA) supporting the energy needs of tissues, but also an ‘endocrine organ’ secreting different so-called adipocytokines or adipokines.30–32 These adipocytokines are polypeptides, mainly produced by VAT in a regulated manner,33 and play a role in insulin resistance (with risk of type 2 diabetes), lipid metabolism, blood pressure, coagulation, fibrinolysis and inflammation (leading to endothelial dysfunction and atherosclerosis) (see Figure 1).24,34
In obesity, adipocytes expand in size because of the deposition of TG.35 This expansion, however, may be limited. It is hypothesised that excessive hypertrophy of the fat cells might create a hypoxic environment within the adipose tissue.36 This could lead to adipocyte death,37 which may then trigger macrophage infiltration.38 Monocyte chemoattractant protein-1 (MCP-1), a chemokine released by adipocytes, is responsible for attracting monocytes into the damaged fat depots.39 Expression and secretion of MCP-1 is known to be elevated in the case of obesity in humans, and is higher in visceral, as compared with subcutaneous, adipose tissue.40
VAT plays a potential role in the pathogenesis of insulin resistance. MCP-1 impairs insulin-stimulated glucose uptake in adipocytes, resulting in a relative resistance to the action of insulin in visceral fat compared with other adipose tissue depots.41–44 Via systemic and local secretion of several adipokines (especially adiponectin and leptin), insulin resistance is influenced.45 Insulin resistance is also influenced by several other systemically and locally secreted adipokines. The elevated FFA levels in visceral obesity induce insulin resistance by the inhibition of glucose transport or phosphorylation, resulting in a reduction of muscle glycogen synthesis as well as glucose oxidation.46,47 The dyslipidaemia associated with abdominal obesity is characterised by elevated TG, reduced high-density lipoprotein (HDL) cholesterol and an excess of small dense low-density lipoprotein (LDL) particles.48 It seems as though visceral adiposity promotes the onset of cardiovascular risk factors, such as high glucose levels, high blood pressure and dyslipidaemia, and this increases cardiovascular disease risk.49
It is well accepted that obesity can be regarded as a state of chronic subclinical inflammation,50,51 and levels of high-sensitivity C-reactive protein (hs-CRP), a marker of low-grade inflammation, have been linked to visceral obesity.24,52–55 Adipose tissue can induce chronic low-grade inflammation by producing pro-inflammatory cytokines such as tumour necrosis factor-α (TNF-α) and interleukin-6 (IL-6).56 The liver is assumed to be the major source of CRP production. It has, however, been suggested that adipose tissue can also be a direct source of CRP. In severely obese patients with a large amount of body fat, adipose tissue might well significantly contribute to the increased circulating CRP levels.57–59 This chronic inflammation plays a role in the development and progression of cardiovascular disease.42 Excess visceral adiposity is probably the missing link between inflammation, cardiovascular disease and type 2 diabetes.60
Because visceral adiposity seems to be an important indicator for metabolic and cardiovascular alterations, it has also been linked to metabolic syndrome, a complex condition characterised by insulin resistance, dyslipidaemia and hypertension.15 In 2005, the International Diabetes Federation even suggested adjusting the definition of metabolic syndrome by including central obesity (measured by waist circumference) as an essential criterion.61 The clinical evidence for the definition of the syndrome and the underlying pathogenesis, however, is the topic of many discussions.<br
Role of Visceral Fat in the Pathogenesis of Non-alcoholic Fatty Liver Disease and Non-alcoholic Steatohepatitis
For a recent review on the pathogenesis of NAFLD/NASH, we refer to the work of Fabbrini et al.62 and to Figure 2.63 In 1998, the ‘two hit’ model of the pathogenesis of NAFLD was proposed. The ‘first hit’ is the excessive accumulation of fat in the liver. This is a consequence of an imbalance between the influx and synthesis of liver lipids on the one hand and their β-oxidation and export on the other hand. The fatty liver becomes sensitive to presumed ‘second hits’ leading to hepatocyte injury, inflammation and fibrosis. These second hits can be oxidative stress (and subsequent lipid peroxidation) and cytokines such as TNF-α, interleukin-8 (IL-8) and transforming growth factor-β (TGF-β).64,65 Emerging data question this ‘simple’ model and suggest that the pathogenesis of NAFLD and NASH is probably much more complex and not yet completely understood.66
The distribution of body fat may be at least as important as total adipose tissue in the development of hepatic steatosis. Central adiposity has been shown to be associated with NAFLD in normal weight, obese and diabetic individuals.13 Van der Poorten et al.67 demonstrated that visceral fat correlates with inflammation and fibrosis in human NAFLD. Patients with NASH have visceral obesity in 48 % of cases versus 31 % of patients with pure steatosis (p=0.005).68 According to Eguchi et al.,69 the severity of fatty liver, evaluated by ultrasonography and CT, was positively correlated with visceral fat accumulation (evaluated by abdominal CT) and insulin resistance in both obese and non-obese subjects, suggesting that hepatic fatty infiltration in NAFLD may be influenced by visceral fat accumulation regardless of body mass index (BMI). A strong association was found between visceral fat accumulation and liver steatosis in morbidly obese women.70 Park et al.1 found that visceral abdominal adiposity (measured by CT) is an independent risk factor for hepatic steatosis in healthy living (disease-free population) liver donors. They concluded that VAT is more important than BMI or obesity itself for hepatic steatosis in men and women. We recently demonstrated a correlation between VAT (measured by CT) and liver tests in an obese population.72 Visceral adiposity has also been shown, together with insulin resistance, to be an independent predictor of the presence of a steatosis-associated increase in portal pressure.73 Visceral adiposity is also an important risk factor for paediatric NAFLD.74 Based on all these data, visceral adiposity is currently considered to be a major contributor to fatty liver, especially in the insulin-resistant state. Some evidence even suggests that visceral adiposity is more influential than body mass in terms of predicting the presence of fatty liver.75
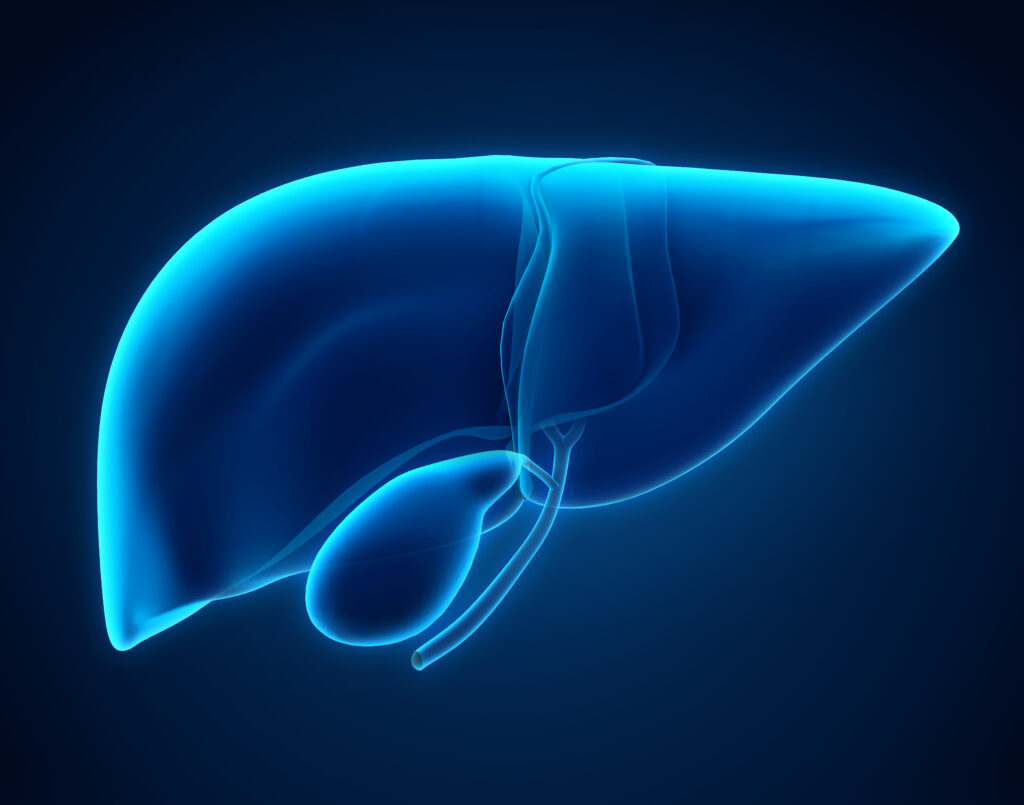
The mechanisms linking VAT and the liver are currently poorly understood. The drainage of the venous blood of the gastrointestinal system, including the VAT, via the portal system to the liver represents a unique anatomical link between the two. Via the portal vein, VAT can directly influence the liver. NAFLD-induced changes in liver haemodynamics might inversely influence VAT.76,77 FFA flux, insulin resistance and adipokines are, along with inflammation and oxidative stress, currently considered to be the main factors in NAFLD pathogenesis related to VAT.
Free Fatty Acid Flux and Alterations in Lipid Metabolism
VAT has greater lipolytic potential than subcutaneous adipose tissue, and the release of FFA from visceral fat directly into the portal circulation creates a first-pass effect. Serum FFA derived from VAT by lipolysis are the main source of hepatic TG in NAFLD, although hepatic de novo lipogenesis and dietary fat supply contribute to the pathogenesis of NAFLD.78 Increased FFA concentrations, in turn, are considered a major mediator of insulin resistance. In contrast, FFA flux and concentrations in individuals with predominantly lower body obesity tend to be normal, regardless of BMI. Therefore, patients with central obesity are typically insulin-resistant, and more commonly present with NAFLD than patients with lower-body obesity.12,79 It appears, however, that visceral fat is a better predictor for insulin resistance and liver dysfunction than BMI.20
Excessive intrahepatic triglyceride (IHTG) content in obese subjects is associated with alterations in both adipose tissue and hepatic lipid metabolism: subjects with NAFLD have increased rates of adipose tissue TG lipolysis and hepatic very low-density lipoprotein (VLDL)-TG secretion. Fabbrine et al.80 showed that the increase in VLDL-TG secretion was caused by an increased incorporation of non-systemic fatty acids, presumably from lipolysis of intrahepatic and intra-abdominal fat and de novo lipogenesis, into VLDL. These data hence suggest that increased IHTG content is not simply a marker of altered hepatic metabolic function, but that it is directly involved in the pathophysiology of NAFLD. Moreover, the increase in VLDL-TG secretion, which is the major source of circulating TG, is probably responsible for the increase in serum TG concentrations commonly observed in patients with NAFLD. The dissociation in VLDLTG and VLDL-apolipoprotein B100 (apoB100) kinetics suggests that a failure to increase adequately the secretion rate of apoB100, which provides the framework for TG incorporation into VLDL, limits the liver’s capacity to export TG.
Insulin Resistance
Insulin resistance is thought to be inevitably linked with the pathogenesis of NAFLD.81 Obesity, type 2 diabetes and hyperlipidaemia are associated with insulin resistance and are often present in patients with NAFLD. There are even insulin-resistant patients with NAFLD who are not obese and have a normal glucose tolerance.68 Insulin resistance classically involves multiple sites: muscle, adipose tissue and the liver. The primary site of insulin resistance in NAFLD, however, is the subject of debate. Is the initial resistance in the periphery (skeletal muscle and adipose tissue) or in the liver?82 Insulin has predominantly anabolic effects on glucose and fat metabolism by promoting glucose uptake, glycolysis and glycogen synthesis in skeletal muscle, by promoting triglyceride synthesis and storage (through inhibition of lipoprotein lipase) in adipose tissue and by inhibition of glycogenolysis and gluconeogenesis in the liver and release of glucose from the liver.83 Insulin resistance, therefore, decreases glucose uptake and utilisation in muscle. In adipose tissue, lipolysis is not adequately suppressed by insulin, with subsequent release of glycerol and non-esterified fatty acids (NEFA) into the circulation. In the liver, insulin resistance is responsible for the overproduction of glucose despite fasting hyperinsulinaemia.18
The metabolic effect of peripheral insulin resistance, partially mediated by decreased plasma adiponectin levels, includes fatty acid flux from adipose tissue to the liver and induces the accumulation of fat in the liver. Elevated plasma glucose can further increase hepatic fat content through multiple pathways, resulting in an overproduction of VLDL-1 particles and leading to the characteristic dyslipidaemia associated with type 2 diabetes.84,85 Molecules such as TNF-α, fatty acids and others appear to interfere with the insulin signalling pathway. The effects of insulin resistance in muscle and adipose tissue interact with the compensatory hyperinsulinaemia on tissues that remain insulinsensitive.
This causes changes in lipid metabolism, such as enhanced peripheral lipolysis, increased hepatic uptake of FFA, and increased hepatic triglyceride synthesis. The influx and neosynthesis of FFA are more important than FFA oxidation and triglyceride secretion, resulting in an accumulation of fat in the liver. Adipose tissue insulin resistance is even associated with increased liver fat content independently of obesity in humans.80,86,87 This hepatic fat subsequently contributes to an impaired glucose metabolism and insulin sensitivity within the liver.3,11,18 Recent data indicate that hyperinsulinaemia is probably the consequence of, rather than a cause of, NAFLD.78
Adipocytokines
Adipocytokines are likely to be involved in the pathogenesis of NAFLD since they are secreted from both adipose tissue and the liver. For several adipocytokines, such as leptin, adiponectin, TNF-α, retinol-binding protein-4 (RBP4) or fetuin-A, a crucial role in the development and progression of fatty liver has been suggested. Dysregulation of adipocytokines may represent an important mechanism linking increased fat mass in obesity with the development of fatty liver disease.88,89 Cytokines are involved in the recruitment and activation of Kupffer cells (resident hepatic macrophages) and are responsible for the transformation and perpetuation of hepatic stellate cells to the myofibroblastic phenotype.32,90
TNF-α and IL-6, two important pro-inflammatory cytokines, are known to be elevated in obesity and NAFLD. TNF-α, together with IL-6 and chemokines, mediates macrophage infiltration which causes inflammation of adipose tissue. This leads to insulin resistance and dysregulation of the secretion of adipokines.91–93
Hypoadiponectinaemia is considered to be involved in the aetiology of hepatic steatosis independently of VAT content, and is considered to be an important factor in the progression of fibrosis.94 Adiponectin may protect the liver from inflammation via direct antagonism of TNF-α.89 Adiponectin concentrations inversely correlate with fat mass and are downregulated in obesity and type 2 diabetes. Adiponectin exerts insulin-sensitising effects in the liver, skeletal muscle, and adipose tissue. In experimental NASH, administration of adiponectin ameliorated necroinflammation and steatosis, partly via inhibition of TNF-α.95 Adiponectin provides signals that are conveyed to adipose tissue, sparing the liver and muscle, and improves insulin sensitivity even in spite of adipose tissue expansion.96 These actions are similar to those induced by thiazolidinediones, which also increase adiponectin levels.97
Secretion of leptin is proportional to fat mass and provides anti-obesity signals, regulating food intake, sympathetic tone and energy expenditure in conditions of energy excess through hypothalamic pathways. Obese patients have elevated levels of leptin, suggesting that they are resistant to the action of this adipokine.98 Mouse models suggest that leptin prevents the development of fatty liver, both indirectly, through central neural pathways, and directly via hepatic activation of adenosine monophosphate-activated protein kinase (AMPK).99,100 Patients with obesity have a fatty liver despite elevated leptin levels, suggesting the presence of hepatic leptin resistance. A role for nutrients has been recently suggested in this disturbance, because fructose induces hyperleptinaemia and hepatic leptin resistance.101 Leptin resistance can also occur because of increased levels of Suppressor of cytokine signalling-3 (SOCS3), which impairs post-receptor signalling and leads to reduced AMPK activation,102 because of activation of the cannabinoid receptor-1 (CB1),103 or because the soluble leptin receptor is expressed by the liver under the control of insulin.104 Leptin also has a profibrogenic role.105 A lot of research is being conducted on other cytokines which are possibly involved in the pathogenesis of NAFLD. Fetuin-A is a hepatic secretory protein that inhibits insulin action, and is suggested to play an important role in the progression of NAFLD. It could link fatty liver disease to insulin resistance, obesity and its comorbidities. It also lowers expression of adiponectin, inducing low-grade inflammation.106 Adipocyte fatty acid-binding protein (AFABP) is secreted by adipocytes and macrophages and correlates with metabolic syndrome and cardiovascular disease. Elevated AFABP serum concentrations are associated with inflammation and fibrosis in NAFLD. Other cytokines possibly involved in the pathogenesis of NAFLD are resistin, progranulin, chemerin, RBP4, TNF-α converting enzyme (TACE), fibroblast growth factor-21 (FGF21), apelin, visceral adipose tissue-derived serpin (vaspin) and omentin.98
Inflammation and Oxidative Stress
Adipose tissue has been shown to be inflamed in subjects with high, as compared with those with low, liver fat content, independently of obesity. This inflammation is characterised by increased macrophage infiltration and accumulation and with increased gene expression of macrophage markers, such as cluster of differentiation-68 (CD68), MCP-1 and macrophage inflammatory protein-1α.107,108 Many studies show that oxidative stress is an important feature of NAFLD. Increased levels of fatty acids in the hepatocytes provide a source of oxidative stress. In obese patients, reactive oxygen species (ROS) can result from production by the hepatocytes but also by adipose tissue.
Oxidative stress may be, in part, responsible for the progression from steatosis to steatohepatitis and cirrhosis. This could occur by three main mechanisms: lipid peroxidation, cytokine induction and Fas ligand induction. Lipid peroxidation (caused by ROS) of plasma or mitochondrial membranes can lead to cell necrosis or can induce apoptosis. ROS also increase Fas ligand on hepatocytes causing apoptotic cell death. They also increase the production of pro-inflammatory cytokines (TNF-α, IL-6, IL-8, etc.).3,109 Low-grade systemic inflammation occurring in metabolic syndrome links insulin resistance, endothelial dysfunction and cardiovascular disease. This systemic subclinical inflammation is also found in obese people and in subjects with NAFLD.19,110
Not all subjects with simple steatosis evolve to the more progressive inflammatory form of NAFLD. Further progression of NAFLD towards cirrhosis leads to diminished secretory capacity of hepatocytes which may result in decreased levels of cytokines mainly produced in the liver.111 Family studies and inter-ethnic variations in susceptibility suggest that genetic factors may be important in determining disease risk. Polymorphisms in genes controlling lipid metabolism, pro-inflammatory cytokines, fibrotic mediators and oxidative stress may be associated with steatohepatitis and/or fibrosis. Genome-wide scans have identified genes contributing to inherited susceptibility to steatosis; similar approaches will probably identify genes associated with disease progression.112 Ethnic differences in visceral fat are also under evaluation as potential links to understand differences in NAFLD.89
Role of Visceral Fat in the Management of Non-alcoholic Fatty Liver Disease
For a recent review on the treatment of NAFLD, we refer to the meta-analysis of randomised trials by Musso et al.113 It is difficult to attribute the histological and biochemical improvement in NAFLD or NASH by any therapy to a decrease in VAT. Studies mostly report about the change in steatosis and liver enzymes, but these can spontaneously fluctuate over time and often improve as necroinflammation and fibrosis progress. Few well-designed randomised controlled trials with histological endpoints are available. It is also important to distinguish between different action sites of the therapy. There can be an effect of the therapy on the amount of total body fat or on the amount of VAT and this change in fat depots can have a differential effect on the liver. There can also be a direct effect of a certain therapy on the liver. Since visceral fat seems to play a central role in the pathogenesis of NAFLD, current therapeutic approaches aim at reducing visceral adipocytederived adipokines and FFA overflow to the liver by weight loss and insulin sensitisers.67,114
Weight Reduction through Lifestyle and Pharmacological Intervention
It is noteworthy that the liver seems to be able to mobilise its fat rapidly. It was found that lifestyle changes, comprising healthy eating habits and regular exercise, reduce liver transaminases and decrease liver fat content.115,116 The degree of fatty infiltration usually decreases with weight loss in most patients, although the degree of necroinflammation and fibrosis may worsen. The rate of weight loss is therefore important and may have a critical role in determining whether liver histology will improve or worsen. In patients with a high degree of fatty infiltration, rapid weight loss may promote necroinflammation, portal fibrosis and bile stasis. Rapid weight loss is of concern in patients choosing a very low-calorie diet (VLCD) or bariatric surgery.2
Currently the only anti-obesity drug on the market is Orlistat, a lipase inhibitor, which reduces the absorption of dietary fat by 30 %. Several studies have demonstrated that this agent reduces weight in obese adults and improves metabolic risk factors.117–119 Use of a lipase inhibitor also improves serum alanine aminotransferase (ALT) levels and steatosis (diagnosed by ultrasound and confirmed by liver biopsy) more than lifestyle modification alone.120–122 Orlistat use is generally well tolerated, with gastrointestinal adverse events (such as fatty and oily stool, faecal urgency and oily spotting) being the most commonly reported effects.121,123,124 The drug has been approved as an over-the-counter 60 mg formulation.
A lot of (promising) research was conducted in the area of the endocannabinoid system, a system that contributes to the physiological regulation of energy balance, food intake, lipid and glucose metabolism through both central and peripheral effects.125 This system consists of endogenous ligands and two types of G-protein-coupled cannabinoid receptors (CB1 and CB2). CB1 is located in numerous organs involved in the regulation of energy homoeostasis, including the brain, adipose tissue, the liver, muscle and the gastrointestinal tract.126 Rimonabant, a selective CB1 blocker, produces clinically meaningful weight loss and additional improvements in waist circumference, lipid concentrations and insulin resistance.127 Animal studies demonstrate that rimonabant may play a hepatoprotective role and suggest that this CB1 receptor antagonist potentially has clinical applications in the treatment of obesity-associated liver diseases and related features of metabolic syndrome.128 Selective CB1 antagonists may even help prevent the development of fatty liver in the presence of a high-fat diet.129 A study conducted in diet-induced obese mice shows that a reduction in the CB1-mediated endocannabinoid system activity in visceral fat, by treatment with the CB1-specific antagonist rimonabant, is associated with a normalisation of adipocyte metabolism, which may be a determining factor in the reversion of liver steatosis.130 Whereas the benefits of rimonabant on cardiometabolic profile and hepatic steatosis emerged, its safety and histological benefit in NASH are unknown. Concerns about depression, anxiety and suicide risk led the Food and Drug Administration to deny drug approval in the US.113 Rimonabant was approved by the European Agency for the Evaluation of Medicinal Products (EMEA) for the treatment of obesity, and has been available in Europe, but has been taken off the European market since October 2008.
Weight Reduction through Surgery
Bariatric surgery is considered to be an effective treatment option in some NAFLD patients with severe obesity or with concomitant obesity-associated disorders.131 A study by Dixon et al. examined the effect of adjustable gastric banding on the histological features of NAFLD and on plasma aminotransferase levels. There were improvements in aspartate aminotransferase (AST), ALT, γ-glutamyl transpeptidase (GGT), lobular steatosis, inflammation and fibrosis between baseline and follow-up.132 Several studies with gastric bypass procedures show a significant improvement in glycaemia, glycated haemoglobin (HbA1c) and lipid profiles. Furthermore, Roux-en-Y gastric bypass (RYGB) results in a significant improvement in the histological features of NAFLD and NASH.133–137 There is, however, no evidence that these effects are due to a decrease in VAT. Surgical resection of the omentum (or part of it) results in a reduction in the amount of visceral fat. When combined with adjustable gastric banding, significant positive and long-term effects are observed in the glucose and insulin metabolic profiles of obese subjects when compared with adjustable gastric banding alone.138 In contrast, Fabbrini et al.139 demonstrated that decreasing VAT through omentectomy, alone or in combination with RYGB surgery, does not improve metabolic function in obese patients. There are no data available from studies of the technique of omentectomy in subjects with NAFLD. Previous studies also report post-operative complications, such as progression of liver disease and subacute liver failure.140 Cases have been reported of severe liver decompensation, and even a need for liver transplantation, after biliopancreatic diversion, possibly due to a progression of steatohepatitis secondary to rapid massive loss of body weight.141,142
Insulin-sensitising Agents
Because of the possible causal nature of insulin resistance, therapeutic interventions aiming at improving insulin sensitivity may be a promising approach to treating NAFLD. Insulin-sensitising agents, such as metformin or thiazolidinediones, may improve the reduced insulin sensitivity in the liver and the periphery, respectively.143 Peroxisome proliferator-activated receptor (PPAR)-γ agonists (or thiazolidinediones) not only increase insulin responsiveness, but have numerous other, potentially beneficial effects, such as lipid-modifying actions, reduction in advanced glycosylation end-product formation and profibrinolytic and antithrombotic actions. Weight gain is, however, a known side effect of this class of drugs. The weight gained during the use of these drugs tends to be peripheral fat, rather than central fat, and therefore it may not be associated with increased risks. This class of drugs also has an effect on NAFLD. Rosiglitazone may cause a significant improvement in histological features, including necroinflammatory changes and fibrosis, with persistence of mild portal inflammation.144 Belfort et al.145 showed that pioglitazone in combination with a hypocaloric diet led to metabolic and histological improvements. In the Diabetes reduction assessment with ramipril and rosiglitazone medication (DREAM) study, rosiglitazone increased the likelihood of regression to normoglycaemia, but also led to a reduction in ALT levels.146 The first Fatty liver improvement by rosiglitazone therapy (FLIRT) trial demonstrated that, in patients with NASH, rosiglitazone improved steatosis and transaminase levels in the first year of treatment.147 The extension trial, FLIRT 2, showed that there was no additional benefit with longer therapy, despite a maintained effect in insulin sensitivity and transaminase levels.148
Normalisation of Adipocytokine Serum Concentrations
Adipokines and their receptors are considered to be novel targets in the pharmacological management of fatty liver disease. The effects of such currently used drugs as thiazolidinediones and metformin depend in part on adiponectin or interfere with its downstream pathways.32,97
Prevention of Supply of Free Fatty Acids to the Liver
VAT plays an important role in the pathogenesis of hepatic steatosis because of its supply of fat to the liver via the portal vein. Sirtuin-1 (SIRT1) could prevent FFAs from being released from VAT. Therefore SIRT1 may be used as a therapy for the management of NAFLD.149